What is TBI?

A traumatic brain injury (TBI) is a serious, potentially life-altering condition that occurs after a sudden blow or jolt to the head. According to the Centers for Disease Control and Prevention, about 2.8 million Americans sustain a TBI every year.
Military service members are at an increased risk for TBIs due to combat and training hazards, including flying debris and exposure to blasts from improvised explosive devices.
How Common is TBI Among Military Personnel?
The TBI Center of Excellence shows that more than 485,500 military personnel were diagnosed with a TBI between 2000 and the second quarter of 2023.
In Wounded Warrior Project® (WWP)’s most recent Annual Warrior Survey, 84% of veterans served by WWP™ reported sustaining a head-related injury or trauma during their military service. Furthermore, 36.5% of warriors surveyed self-reported having a TBI.
The increase in prevalence led VA to classify TBI as a “signature injury” among post-9/11 military service members. However, traumatic brain injuries are often misunderstood, so VA believes the incidence of TBI may be underreported.
What Happens During a TBI?
Some compare a TBI to an internal earthquake of the brain. The aftershocks may affect a person’s physical, cognitive, and mental health, leading to short- and long-term challenges that can impact relationships, social interactions, employment, and self-care.
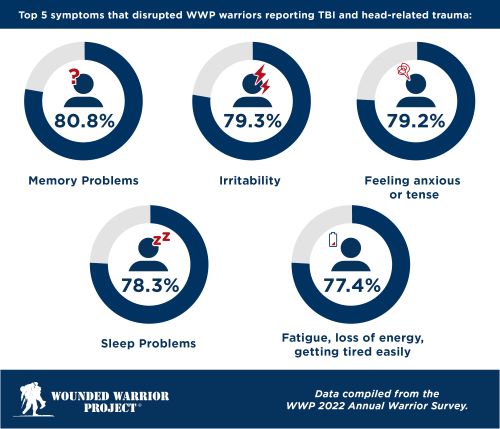
WWP warriors who reported some form of head-related trauma also experienced a negative impact on quality of life. The most common symptoms that began or worsened for warriors after head-related trauma were feeling anxious or tense, having sleep problems, and irritability.
Common Myths About TBIs
There are many misconceptions about traumatic brain injuries. A study commissioned by WWP and conducted by the RAND Corporation looked at the current state of TBI among post-9/11 veterans. The report, published in April 2022, noted that while there has been progress in developing screening and treatments for those with TBIs, gaps remain. Helping warriors and their loved ones better understand these injuries will be beneficial to navigating challenges and improving their quality of life.
Myth: All TBIs result from blows to the head.
Fact: Falls and car accidents are the two most common causes of TBI, but military members have potential exposure to more hazards, whether deployed or not. Many operational or training exercises, including parachuting, mountain climbing, and hand-to-hand combat drills, are physically demanding and may increase the risk of injuries.
Myth: If you don't lose consciousness, it's not a TBI.
Fact: TBIs don't always cause a loss of consciousness. Someone with a mild TBI may not lose consciousness but rather experience significant confusion.
There are several types of TBI:
• Mild: When a person loses consciousness for 30 minutes or less (or doesn't lose consciousness).
• Moderate: If a person loses consciousness for more than 30 minutes but wakes up within 24 hours.
• Severe: A loss of consciousness for 24 hours or longer.
Myth: All TBI symptoms are the same and can only occur immediately after sustaining an injury.
Fact: Every person is different, and so is their injury. Symptoms – and the onset of those symptoms – will vary based on the person, the injury's severity, and the injury's location in the brain. Someone who has a TBI may experience these symptoms:
• Physical: Loss of consciousness, headache, nausea, dilation of pupils, and coordination challenges, including loss of balance or dizziness, fatigue, and problems with speech.
• Sensory: Blurred vision, ringing in ears, sensitivity to light or sound.
• Cognitive and mental: Confusion, disorientation, memory problems, mood swings, depression, anxiety, sleeping more than usual.
People who have more severe trauma may exhibit more profound symptoms, including seizures, worsening headaches, slurred speech, combativeness, and loss of mobility. Symptoms can sometimes emerge weeks, months, or even years after the initial incident. Recognizing delayed symptoms and seeking help remains crucial regardless of the timeframe.
Myth: Mild TBIs are insignificant and do not require attention or treatment.
Fact: A brain injury is significant, even if you don't lose consciousness. The VA’s Office of Research and Development reports that most TBIs are mild – which means you may not lose consciousness at all. A concussion is the most common type of mild brain injury.
Prompt evaluation is important anytime a person has been in a potentially concussive event, as an early diagnosis can lead to improved long-term outcomes. However, reaching out for help is always possible, even if time has elapsed since an injury. An evaluation with a physician, including a review of symptom history, can be valuable in confirming a diagnosis and assessing long-term consequences.
Myth: There is no treatment for veterans with TBIs.
Fact: People with TBI can lead productive and fulfilling lives. Treatment options for TBIs are constantly evolving, and many veterans experience significant improvement with proper medical care, mental health support, and rehabilitation. Dismissing the potential for recovery can discourage veterans from seeking the help they need.
Resources for TBI Care and Research
One of the key recommendations from the WWP/RAND report was the importance of taking advantage of veteran-specific resources to optimize long-term outcomes for veterans.
WWP offers access to clinical programs and care models that provide integrated treatment based on the severity of a veteran’s TBI. Programs also offer services for family members and caregivers.
- WWP’s Independence Program is for the most severely wounded veterans. The program provides care and long-term support services to warriors and their caregivers to help them re-engage in the community and improve their overall quality of life.
- Warrior Care Network® is a partnership with four of the nation’s top medical facilities that provide mental health care for veterans with post-traumatic stress disorder (PTSD) and brain injuries. Warrior Care Network also has workshops and tracks for family members to help them understand and cope with TBI effects while supporting their loved ones.
The RAND report noted the importance of TBI research in improving the overall health and well-being of veterans with TBIs. The VA’s Office of Research and Development has extensive data on advancements, including ongoing research around diagnostics and innovations in care and treatment.
A Warrior's Experience with TBI and PTSD: Signature Injuries Often Confused
“I wish I had known sooner I had a TBI. I think things would have been different, and I could have started healing sooner,” said Eric DeLion, a Marine veteran exposed to multiple attacks and explosions during his time in Iraq.
Although he recalls blasts strong enough to blow out tires and destroy vehicle engines, “us inside, for the most part, didn’t sustain any physical, visual injuries.”

Eric DeLion and his children. Erin is living with a TBI and PTSD, injuries that are often confused.
Unbeknownst to Eric, the impacts caused a traumatic brain injury.
It's a familiar tale among veterans. The signs of TBI can be difficult to detect, especially since symptoms might not show up immediately after injury, and sorting through symptoms can be confusing. Many times, healthcare providers classify a veteran's symptoms as post-traumatic stress disorder, which is also considered a signature injury of post-9/11 era veterans. It can take years to obtain an accurate diagnosis.
Often, PTSD and TBI occur simultaneously. Although they are separate conditions, the symptoms of PTSD and TBI often blend into each other. The effects of TBI may impact the way a person reacts to their PTSD symptoms. Likewise, PTSD can make TBI treatment more complex.
Eric suffered from headaches, short-term memory lapses, and mood swings. He was told his symptoms were related to PTSD and was eventually medically retired.
“It was definitely rough because I wasn’t myself, and it took me a while to adjust to my new normal,” Eric said, noting that having family support and connecting with other veterans at WWP events is a significant part of his journey.
Although Eric has learned various skills over the years to manage his TBI and PTSD symptoms, the father of three still wonders some days how life would have been if he'd gotten an accurate TBI diagnosis sooner.
"I'm not sure how things would be different exactly, but I feel if I could have started working on things sooner, I would have been more comfortable. For instance, I have short-term memory loss. If I had the TBI discovered sooner, I could have learned tricks to strengthen and improve my brain earlier.”
Today, Eric advocates for TBI awareness, reminding other veterans that “it’s OK not to be OK and to seek help.”
“I hope my fellow brothers and sisters in arms find help and know they are not alone,” he said. “Although the wars might not be talked about anymore, we are not forgotten. There are still people and organizations like Wounded Warrior Project that care for us. So, I say never quit and never give up hope!”
Get connected with WWP today or read more about how WWP helps.
Contact: Cynthia Weiss – Public Relations, cweiss@woundedwarriorproject.org, 904.738.2589
About Wounded Warrior Project
Since 2003, Wounded Warrior Project® (WWP) has been meeting the growing needs of warriors, their families, and caregivers — helping them achieve their highest ambition. Learn more.


