Living with Toxic Exposure
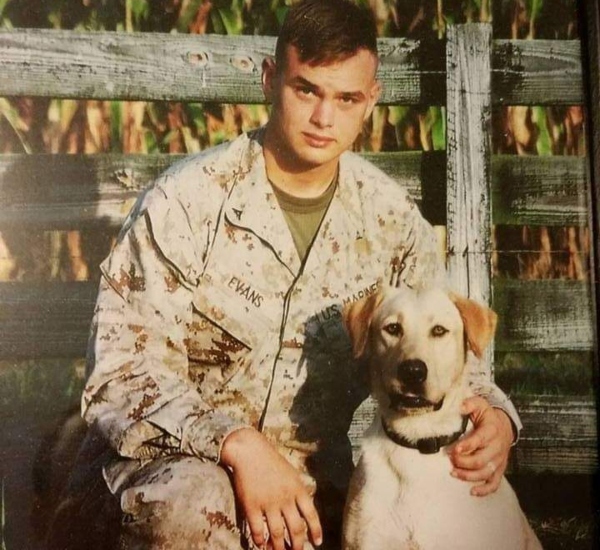
By: Scott Evans, Marine Corps veteran
Exposure to contaminants or other environmental hazards is a major health concern for post-9/11 veterans. To date, more than 200,000 veterans and service members have enrolled in the VA’s Burn Pit Registry – all of whom served on or after 9/11 and were deployed to a base or station where open burn pits were used.
For those seeking treatment for illnesses sustained during military service, the largest barrier for using VA health systems is establishing a service-connected disability.
A WWP warrior shares his story here:
I deployed to Afghanistan twice in five years. The first time was in 2009, and the second was in 2011. As a U.S. Marine Corps combat engineer and dog handler, I was on a team responsible for training military dogs to detect improvised explosive devices (IEDs) as well as implementing the dogs as a counter IED asset. We trained the dogs in burn pits so they would learn to avoid distractions. This simulation was the closest thing we could do in a controlled environment to replicate the environment in Afghanistan. The rationale was if the dogs were able to identify IEDs in burn pits, then they would have fewer problems identifying them in a real-world application.
The burn pits we trained in were around the size of a football field, and in some cases bigger. On any given day, a person could find anything from batteries to old computers to four-wheelers being burned. A lot of the time, there were fires 20 to 30 feet away and you would normally see plumes of smoke.
Throughout both deployments, I developed a nagging cough and chronic sneezing, but at the time it seemed common because we were in the desert and the bases were filled with dust and sand.
Returning Home
I returned home from my last deployment to Afghanistan in November 2011 and was honorably discharged from the Marine Corps in January 2012.
Over the years, a nagging cough and stuffy nose became the norm, but in the spring of 2020, things took a turn for the worse. I started experiencing severe abdominal pain and rapid weight loss. My wife noticed that my eyes started to turn yellow and before I knew it, it was painful to walk and my biceps began to shrink. It was one of the most difficult times of my life.
When I attempted to seek care and enroll at my local VA Medical Center, I was told that I was ineligible since I had never filed a disability claim and it was beyond the five-year eligibility period for combat veterans.
Although I was denied access to healthcare, I was still in need of treatment. My only option was to visit a private doctor. After several visits and seeing multiple specialists, there was still no diagnosis. To add insult to injury, I had a specialist tell me that my condition was due to excessive alcohol use despite my telling them that I consume only one or two drinks a year. One of the most frustrating parts of the process was continuously hearing from doctors, “Don’t worry, we have time.”
In the span of three to four months, I lost around 100 pounds and accumulated around $20,000 in medical bills, yet I still had no idea what was wrong.
All of the money we saved over the years was gone in a matter of months, and as the medical bills piled up, my health rapidly declined. At this point, I started to become discouraged because it seemed like no one cared and no one wanted to or was willing help.
In July, a fellow service member connected me with Wounded Warrior Project, and they stepped in and helped get me through the door at my local VA medical center. Without this, I have no doubt that I would have already passed away. During my first appointment – within 20 minutes of being in the ER, the doctor looked at the scan and told me it was most likely cancer.
The official diagnosis came at the end of July: inoperable pancreatic cancer.
Life After Toxic Exposure
Since being successfully enrolled at VA, I’ve received world-class care. The doctors at VA have a much better understanding of toxic exposures and more importantly, listen to my concerns. For almost six months, I received very aggressive chemotherapy that significantly reduced the cancer activity. My last chemo treatment was at the end of January. I am now on a sustainment drug to allow my body time to recover to prepare for round two with this cancer. The sustainment drug is working for the most part, but we are still seeing around 35% growth in the tumor a month. I need to recover as I am a shell of myself; I currently sit at 155 pounds at 6-foot-3.
Every day is different, but overall, I’m feeling pretty good physically. In March, I started to gain a bit of strength back and I’m able to do some things independently.
As I recover, at times it’s hard to not think of all of the obstacles I had to face to just get the care from the VA and the difficulties to get enrolled in VA. Thankfully, last month there was a significant breakthrough - my claim with the VA was approved, and my cancer is officially considered service-related.
Despite this major victory, it is hard sometimes not to wonder where I would be now if I was able to enroll when my symptoms started in March 2020. Would my prognosis have been better? Would the cancer have been operable? It is what it is, though. We can only focus on what is in front of us and move forward.
My life has mostly remained normal throughout all of this. The company I work with has been exceptional and has arranged for me to continue to work. I am sincerely grateful for that as it helps me have a purpose and something to do during the days. The biggest change to my life is I now only really leave my home to go to my medical appointments.
My wife has been fantastic throughout this in stopping her life to take care of me. She is my best friend. We have been together for 18 years now. One of the biggest things I find myself struggling with is planning. I have always looked toward the future and prepared for it. Now I know I don’t have much time left, and it is frustrating because I still find myself making plans for years ahead that unfortunately, I won’t be here for. I have come to terms with my mortality when I enlisted and dying isn’t something I have ever feared but leaving behind my wife is something I find very unfair. I wish I would be here to take care of her and watch her grow old.
Read “Wounded Warrior Project Supports Introduction of the True Cost of War Recognition Act”